Blogue
Bubbles exploring the brain


Spatiotemporal Ultrasound Localization Microscopy can reveal a whole world hitherto inaccessible to medical teams. On the right, the image of a mouse brain without image processing, and on the left, after microbubbles localization (Photo: Chloé Bourquin)
In a laboratory in the Lassonde pavilion, a Polytechnique Montréal team is refining a medical imaging technique that could detect the warning signs of Alzheimer's or Parkinson's disease, critically, several years before the onset of symptoms. It’s a new tool that relies on millions of bubbles, an ultrasound, and gigabyte video sequences.
With each beat, the heart pumps blood with enough pressure that it could damage organs. It's worth noting that at 130 kPa - or 120 mm of mercury - each pulse displaces blood with air pressure equivalent to that contained in a car tire.
Fortunately for us, arteries and other blood vessels absorb some of this energy as they dilate, so instead of surging like a torrent through our bodies, blood gradually slows down. Blood leaves arteries - the body's highways - to gain access to smaller and smaller blood vessels, until it reaches capillaries. Capillaries are vessels which are 3 to 10 micrometers in diameter - 5 to 10 times thinner than a hair. There, heartbeats are almost imperceptible.
The problem is that over time our bloodvessels become less elastic, their ability to absorb the heart's pulsing wave decreases, and blood flows forcefully into the smallest vessels. At the end of the network, capillaries suffer from the onslaught; their cell monolayer breaks down and as a result, tissues are less well supplied with blood and the cells die because they don't have access to adequate nutrients.
According to various studies, this very phenomenon could be involved in the development of neurodegenerative diseases such as Alzheimer's or Parkinson's. It can take these, and other long-term illnesses up to 10 to 15 years to manifest symptoms, and these are diseases that modern medicine is currently unable to diagnose using imaging techniques - but, a Polytechnique Montreal team is working on a solution.
bubbles and ultrasound

|
Professor Jean Provost (Photo : Polytechnique Montréal)
|
In his laboratory in the Lassonde Building, the Department of Chemical Engineering’s Professor Jean Provost is participating in the development of a new vascular imaging technology. This approach - that goes by various names including "ultra-dynamic ultrasound imaging" or "ultrasound localization microscopy" - is unique in that could potentially detect the first signs of certain neurodegenerative diseases.
Just as an ultrasound does, this new technique permits the visualization of what is happening a mere few centimeters under the skin, but what differentiates it, is that the ultrasonic probe detects fine bubbles that have previously been injected into the patients' blood circulation. Unlike a traditional ultrasound, we're not trying to determine an in-utero baby's health, or the state an appendix – we’re looking much deeper.
"We already use the same microbubbles as a contrast agent in medical imaging - they're perfectly harmless. We inject millions of them into the patients' blood, then we detect them one by one through the skin with an ultrasonic probe," explains Professor Provost.
Using the above approach, the desire is to measure the "pulsatility" of blood flow, the back and forth due to the variation in blood pressure observed between each heartbeat. The ultrasound probe follows each bubble's movement at a given location.
Results garnered from the above process not only generate a blood network map, but also a video - the 'added value' that this technique brings. Professor Provost confides, “We're not interested in anatomical detail, we’re interested in the movement of bubbles in the vessels."
A snapshot of... ultradynamic ultrasound imaging |
|
A team from the Laboratoire Physique pour la Médecine (ESPCI Paris-PSL, Inserm, CNRS) also works on spatiotemporal ultrasound localization microscopy (Crédit: YouTube) Ultradynamic ultrasound imaging hasn't yet been adopted for use in hospitals around the world, unlike its predacessors, magnetic resonance imaging (MRI) or positron emission tomography (PET scan). Yet, it nevertheless remains the only technique with the potential to probe in-depth, the microvascularization of tissues. A French team recently demonstrated that it can be considered in humans; their story can be found on YouTube: |
One Netflix movie per second
Yet before being able to use this tool routinely in human patients, there’s still some optimization work to be done. This is where Professor Provost's team comes in: "The main challenge is to detect enough microbubbles within a reasonable amount of time to form a complete vascular map," notes the Professor.
“If we inject too many microbubbles, then we can't detect them individually, whereas if we inject too few, the time required to capture the images becomes too long. This problem adds to the challenge of managing the volume of images captured by the probe."
The bubble-based ultrasound captures 2,000 to 5,000 frames every second - roughly the equivalent of a high-resolution movie downloaded from Netflix (around 1 GB). For a 10-minute video, it's closer to a terabyte (10TB) - the equivalent of the entire 10 seasons of Friends!
a helping hand from ai
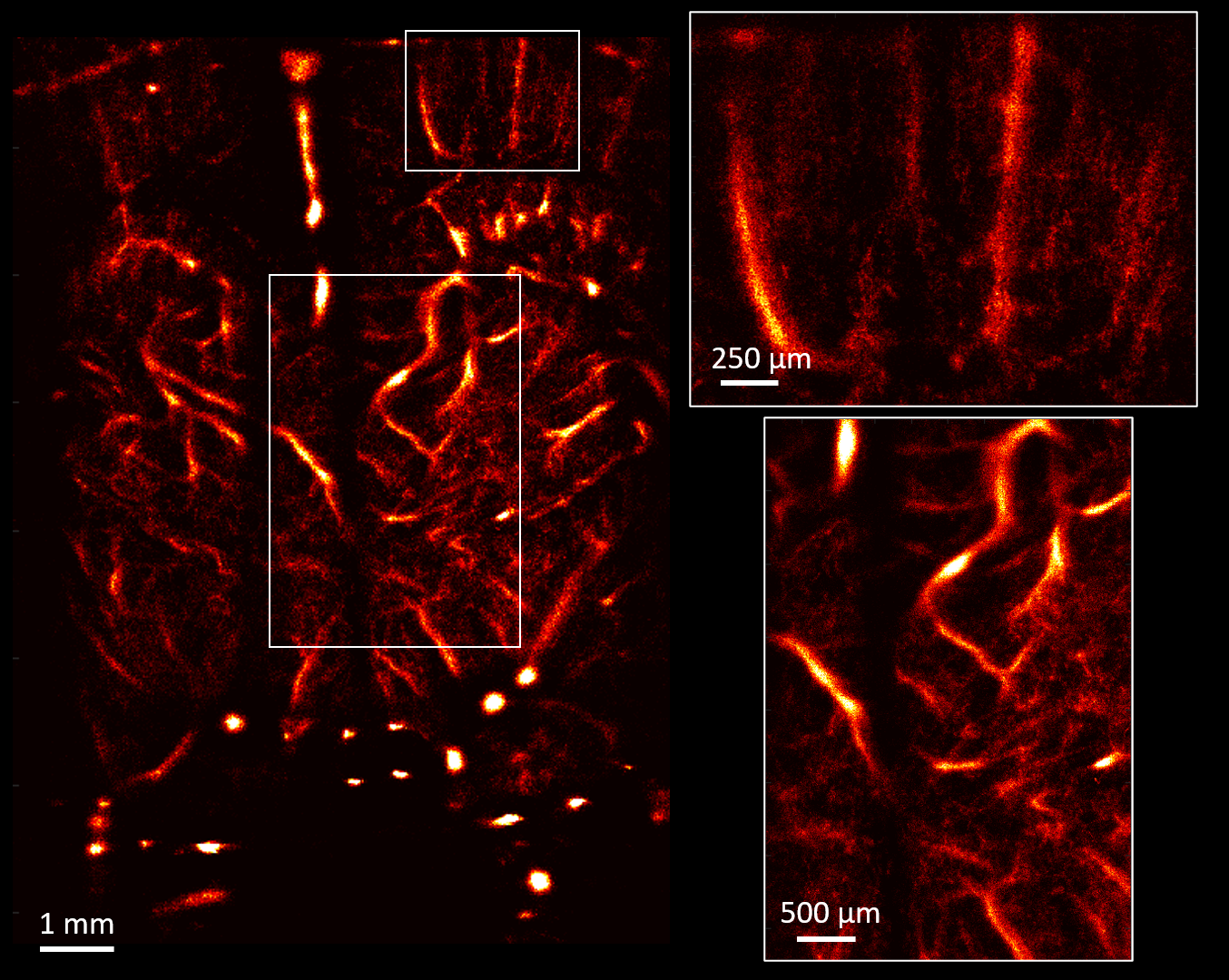
By analyzing over 150,000 images captured in 4 minutes, Professor Provost's team generated the above image that shows blood vessels in a rat's brain. It's estimated that the voyage of over 5,000,000 bubbles was followed during the procedure. (Photo : Chloé Bourquin)
A reasonable balance of bubbles needs to be found, and to identify it, Professor Provost's team are relying on artificial intelligence. “We developed a new neural network architecture tool that we trained using realistic simulations based on two-photon microscopy,” explains the researcher.
“With this approach, we can drastically increase the concentration of bubbles while at the same time reduce the acquisition time to obtain the same information."
In other words, the algorithm tool learned to measure pulsatility by observing a cloud of bubbles that would be indistinguishable for the vast majority of us - an exploit whose details were recently published in a recent scientific article in the journal IEEE Transactions on Medical Imaging.
The researcher and team are now testing their algorithm on images acquired from blood vessels around a mouse's heart - and therein lies another niche where this imaging technique could prove useful, according to Professor Provost. With this new tool, one could find out if small blood vessels in the myocardium wall are blocked or not, or determine whether an aneurysm is likely to occur soon.
We're... recruting! |
 The lab is recruiting! Professor Provost and Dr. Hélène Girouard’s team is recruiting, and are on the lookout for a doctoral student or a postdoctoral fellow for a related project. For more information, see the folliwing link. |
Learn more
Professor Jean Provost expertise;
Provost Ultrasound Lab's website;
Chemical Engineering Department's website;
IEEE Transactions on Medical Imaging's scientific article





Comments
Commenter
* champs obligatoire